The attachments to the deleted claim cannot be used to process the new claim. Intermittent, meaning they do not occur continuously but instead comes and goes at intervals. If you hired your employee on or before Nov. 6, 1986, and still employ that person, you are generally not required to complete Form I-9 for that employee. Review the report weekly and submit a new, corrected claim if needed. You will receive important documents from us generally within two weeks after you file for unemployment. Otherwise, be aware that your insurance company may request additional documents, such as your medical history records to support your claim, so its important to stay on top of the process. Here are some basic steps to help you get started with billing. Tip:The fastest way to apply is throughUI Online. Medical coders and billers use this form on a daily basis. If you lost your job or had your hours reduced, you may beeligiblefor unemployment.  At the very top of the claim form, on the right hand side, is a section for the patient's insurance claims address.
At the very top of the claim form, on the right hand side, is a section for the patient's insurance claims address.  If Medicare denied a service, Medicaid will not pay for it on the Medicare crossover" claim. Nebraska Medicaid uses national codes for reporting on the electronic remittance advice and other reports. You can also send multiple claims for different patients to the same insurance at the same time. If you need to change the information on a paid claim or request reconsideration on a denied claim, you must submit an adjustment request. Have the Medicaid claim number (from the Medicaid remittance advice) ready. I am new to billing Medicaid. Do I need to submit a claim to Medicaid? nathaniel joseph yahoo The report mailed to your payment address and is sent only if you have claims in process over 30 days. Claims that have been in process for less than 31 days will not appear on the report. If it has been forwarded, please do not send another claim. If youre noteligible for unemployment, you may be eligible forDisability InsuranceorPaid Family Leave. Nebraska uses national code sets for procedures, procedure code modifiers, diagnosis and most other claim information. Contract to do a job according to their own means and methods. Review our. Claims are returned if they are missing information required for entry into the Medicaid claims processing system.
In these cases, you will need to submit a new claim. Underneath the address is a complicated set of numbered and lettered boxes. If you are unable to verify your identity through ID.me when applying online, you will need to file a claim by phone, fax, or mail. During this time, they are referred to as instream," pending" or not finalized.". Information on all employers you worked for during the past 18 months, including name, address (mailing and physical location), the dates of employment, gross wages earned, hours worked per week, hourly rate of pay, and the reason you are no longer working. You may be trying to access this site from a secured browser on the server. hbbd```b``>"H mXDtA$B0 Keep an extra copy of the competed claim form as well as your collected receipts in case there is a complication with your claim. annular vail saturn What should I do? Cant find what you are looking for? The standard Form I-9 must be used for employees hired on or after Nov. 28, 2011. The remittance advice includes information to identify the claim, the Medicaid claim number, payment amount and denial reasons. All employers must complete and retainForm I-9, Employment Eligibility Verification, for every person they hire for employment after Nov. 6, 1986, in the U.S. as long as the person works for pay or other type of payment. Keep an eye on your calendar, bearing in mind the claim date that your insurance company gave you when you called. 0
Form 1099G tax information is available for up to five years throughUI Online. Do not send us a claim unless the service you provided is one that is never covered under Medicare. You are unable to perform your normal work duties because you are sick or quarantined due to. Keep in mind that each form should have instructions for completing the form and directions on how and where to send it, but if you have questions simply contact your insurance company. Log in to allow ID.me to share your identity information with the EDD. hair mods cullen awards game The first set of information is the patient data, including: Because the patient isn't always the insurance subscriber, but instead a child, spouse, or other dependent on the policy, this is a necessary relationship to include. In this case, please do not submit a new claim. It's so that the insurance company can determine whether or not the dependent is covered under the insurance policy. A notice of these deleted claims will be mailed to the address on your claim. Take the necessary steps to make sure your unemployment benefits are not delayed or denied. Register and create an accountwith Benefit Programs Online. This page was not helpful because the content: Questions and Answers Related to COVID-19, Completing Section 1, Employee Information and Attestation, Completing Section 2, Employer Review and Attestation, Completing Section 3, Reverification and Rehires, Form I-9, Employment Eligibility Verification, Commonwealth of the Northern Mariana Islands (CNMI), Section One: Employee Information and Attestation, Section Two: Employer or Authorized Representative Review and Verification, Section Three: Reverification and Rehires, Employees in the Commonwealth of the Northern Mariana Islands, Employees from the Federated States of Micronesia, the Republic of the Marshall Islands, and Palau, Temporary Protected Status (TPS) beneficiaries, Employees resuming their job after a temporary break in employment, Handbook for Employers M-274, Guidance for Completing Form I-9, Employment Eligibility Verification Form, Status of Citizens of the Republic of Palau Factsheet, Status of Citizens of the Federated States of Micronesia and the Republic of the Marshall Islands Factsheet, Immigration and Customs Enforcement IMAGE Program, DHS Office for Civil Rights and Civil Liberties (CRCL), Immigrant and Employee Rights Section (IER), How and when to complete the three sections of the form, What to do if you think a document looks fraudulent, How to better ensure that the employer is hiring a legal workforce, Individuals hired on or before Nov. 6, 1986, who are continuing in their employment and have a reasonable expectation of employment at all times. This process can reimburse you for any visits youve paid for out-of-pocket and ensure your medical bills are paid as promptly as possible. Claim adjustment requests that are approved and result in payment changes are reported on the Medicaid remittance advice. Adjustment requests must be clearly marked and contain the following information: Client ID, provider ID, date of service, Medicaid claim number and the reason the adjustment is being requested. Determine the hours during which the work is to be done. 636 0 obj
<>
endobj
Invest in facilities to do all or part of the work. You should correct the claim or submit a new claim within six months from the date of service. If you provide Medicare-covered services to dual-eligible clients, remember that Medicare will automatically send(crossover") your claims to us for processing and payment of coinsurance and deductible. If your claim does not appear on the report as expected, or if your claim was listed on a prior report and is no longer on the report, the claim either completed processing (check your Medicaid remittance advice) or was deleted (check your deleted Medicaid claims report). Remember, if your claim was returned, rejected or deleted, and you submitted a new claim, the 30-day timeframe starts again with receipt of the new claim.
If Medicare denied a service, Medicaid will not pay for it on the Medicare crossover" claim. Nebraska Medicaid uses national codes for reporting on the electronic remittance advice and other reports. You can also send multiple claims for different patients to the same insurance at the same time. If you need to change the information on a paid claim or request reconsideration on a denied claim, you must submit an adjustment request. Have the Medicaid claim number (from the Medicaid remittance advice) ready. I am new to billing Medicaid. Do I need to submit a claim to Medicaid? nathaniel joseph yahoo The report mailed to your payment address and is sent only if you have claims in process over 30 days. Claims that have been in process for less than 31 days will not appear on the report. If it has been forwarded, please do not send another claim. If youre noteligible for unemployment, you may be eligible forDisability InsuranceorPaid Family Leave. Nebraska uses national code sets for procedures, procedure code modifiers, diagnosis and most other claim information. Contract to do a job according to their own means and methods. Review our. Claims are returned if they are missing information required for entry into the Medicaid claims processing system.
In these cases, you will need to submit a new claim. Underneath the address is a complicated set of numbered and lettered boxes. If you are unable to verify your identity through ID.me when applying online, you will need to file a claim by phone, fax, or mail. During this time, they are referred to as instream," pending" or not finalized.". Information on all employers you worked for during the past 18 months, including name, address (mailing and physical location), the dates of employment, gross wages earned, hours worked per week, hourly rate of pay, and the reason you are no longer working. You may be trying to access this site from a secured browser on the server. hbbd```b``>"H mXDtA$B0 Keep an extra copy of the competed claim form as well as your collected receipts in case there is a complication with your claim. annular vail saturn What should I do? Cant find what you are looking for? The standard Form I-9 must be used for employees hired on or after Nov. 28, 2011. The remittance advice includes information to identify the claim, the Medicaid claim number, payment amount and denial reasons. All employers must complete and retainForm I-9, Employment Eligibility Verification, for every person they hire for employment after Nov. 6, 1986, in the U.S. as long as the person works for pay or other type of payment. Keep an eye on your calendar, bearing in mind the claim date that your insurance company gave you when you called. 0
Form 1099G tax information is available for up to five years throughUI Online. Do not send us a claim unless the service you provided is one that is never covered under Medicare. You are unable to perform your normal work duties because you are sick or quarantined due to. Keep in mind that each form should have instructions for completing the form and directions on how and where to send it, but if you have questions simply contact your insurance company. Log in to allow ID.me to share your identity information with the EDD. hair mods cullen awards game The first set of information is the patient data, including: Because the patient isn't always the insurance subscriber, but instead a child, spouse, or other dependent on the policy, this is a necessary relationship to include. In this case, please do not submit a new claim. It's so that the insurance company can determine whether or not the dependent is covered under the insurance policy. A notice of these deleted claims will be mailed to the address on your claim. Take the necessary steps to make sure your unemployment benefits are not delayed or denied. Register and create an accountwith Benefit Programs Online. This page was not helpful because the content: Questions and Answers Related to COVID-19, Completing Section 1, Employee Information and Attestation, Completing Section 2, Employer Review and Attestation, Completing Section 3, Reverification and Rehires, Form I-9, Employment Eligibility Verification, Commonwealth of the Northern Mariana Islands (CNMI), Section One: Employee Information and Attestation, Section Two: Employer or Authorized Representative Review and Verification, Section Three: Reverification and Rehires, Employees in the Commonwealth of the Northern Mariana Islands, Employees from the Federated States of Micronesia, the Republic of the Marshall Islands, and Palau, Temporary Protected Status (TPS) beneficiaries, Employees resuming their job after a temporary break in employment, Handbook for Employers M-274, Guidance for Completing Form I-9, Employment Eligibility Verification Form, Status of Citizens of the Republic of Palau Factsheet, Status of Citizens of the Federated States of Micronesia and the Republic of the Marshall Islands Factsheet, Immigration and Customs Enforcement IMAGE Program, DHS Office for Civil Rights and Civil Liberties (CRCL), Immigrant and Employee Rights Section (IER), How and when to complete the three sections of the form, What to do if you think a document looks fraudulent, How to better ensure that the employer is hiring a legal workforce, Individuals hired on or before Nov. 6, 1986, who are continuing in their employment and have a reasonable expectation of employment at all times. This process can reimburse you for any visits youve paid for out-of-pocket and ensure your medical bills are paid as promptly as possible. Claim adjustment requests that are approved and result in payment changes are reported on the Medicaid remittance advice. Adjustment requests must be clearly marked and contain the following information: Client ID, provider ID, date of service, Medicaid claim number and the reason the adjustment is being requested. Determine the hours during which the work is to be done. 636 0 obj
<>
endobj
Invest in facilities to do all or part of the work. You should correct the claim or submit a new claim within six months from the date of service. If you provide Medicare-covered services to dual-eligible clients, remember that Medicare will automatically send(crossover") your claims to us for processing and payment of coinsurance and deductible. If your claim does not appear on the report as expected, or if your claim was listed on a prior report and is no longer on the report, the claim either completed processing (check your Medicaid remittance advice) or was deleted (check your deleted Medicaid claims report). Remember, if your claim was returned, rejected or deleted, and you submitted a new claim, the 30-day timeframe starts again with receipt of the new claim.  How do I submit one?"). Familiarize yourself with your Medicaid provider handbook. Consider submitting claims electronically. Also included here is a section where you can indicate whether or not the medical visit was due to an accident, which may be covered under worker's compensation or vehicle insurance. The second half of the CMS 1500 claim form is the section labeled Physician and Supplier Information. Remember to check before the 90-day time limit expires. Claims for certain services require special documentation. This usually takes two to three weeks. Straight, simple and to the point five easy steps to help you efficiently file a health For an example and explanation of this report, see 471-000-128 (for CMS1500, dental, nursing facility turnaround and electronic 837 practitioner and dental claims) and 471-000-129 (for CMS1450 and electronic 837 institutional claims). You do not need to reapplyif you did not earnenough wagesin the last 18 months to establish a new claim. If your company merges with another company, you may need to complete Form I-9 for an employee of the newly acquired company who was originally hired on or before Nov. 6,1986.Learn more about mergers and acquisition. An independent contractor is not considered an employee for Form I-9 purposes and does not need to complete Form I-9. The claim form only allows enough room for four diagnoses. If you submit electronic claims, you will also need to review the implementation guides and Nebraska Medicaid companion guides on our EDI web page, which includes frequently asked questions and EDI report examples. To file a claim you need to first obtain an itemized bill from your doctor or medical provider. Handbooks are published on the DHHS website. You cannot be paid for weeks of unemployment after your benefit year ends, even if you have a balance on your claim. Form I-9, Employment Eligibility Verificationconsists of three sections: IN THESE SECTIONS YOU CAN ALSO FIND MORE INFORMATION ABOUT: You are required to complete and retain a Form I-9 for every employee you hire for employment in the United States, except for: Federal law prohibits individuals or businesses from contracting with an independent contractor knowing that the independent contractor is not authorized to work in the U.S. var y=x.getYear() A contact list is available online. In theCommonwealth of the Northern Mariana Islands (CNMI), employers have had to complete Form I-9 CNMI for every employee hired for employment in the CNMI from Nov. 28, 2009 to Nov. 27, 2011. This Google translation feature, provided on the Employment Development Department (EDD) website, is for informational purposes only. The bulletins that apply to the services you provide are included with your provider handbook. document.write(y+1900), If you're interested in mastering the CMS 1500 claim form, we recommend the ebook, Back from CMS 1500 Claim Form Tutorial to Medical Billing Tutorials. For instructions and a printable form, see form MS-84. You need to take time off work to care for a seriously ill child, parent, parent-in-law, grandparent, grandchild, sibling, spouse, or registered domestic partner. You paid into the State Disability Insurance program (noted as CASDI on paystubs), via taxes. Rejected claims are reported on the electronic claim activity report" sent to your electronic submitter/clearinghouse. Claims that have been entered into the Medicaid claims processing system go through a series of edits and reviews to determine if the claim is payable. If you have general questions or need help with account registration, password resets, your EDD Account Number, or how to use UI Online, contact us at 1-800-300-5616 from 8 a.m. to 5 p.m. (Pacific time), Monday through Friday, except state holidays. It will assist DHHS in moving toward a more efficient payment system. It looks like your browser does not have JavaScript enabled. This report lists your paper and electronic claims in process that were received at least 30 days prior to the report date. Be sure to ask them if there are any additional documents that may need to be sent and how long until you expect for the claim to be paid. 661 0 obj
<>/Filter/FlateDecode/ID[<3E75FE2F058F014AB90C1F15A97E2C47>]/Index[636 46]/Info 635 0 R/Length 119/Prev 290857/Root 637 0 R/Size 682/Type/XRef/W[1 3 1]>>stream
These claims can be paid or denied (paid at $0). You must meet alleligibility requirementswhen filing for unemployment and certifying for benefits. In this case it's necessary to include this information to make sure that the claim is paid correctly by the primary insurance. Direct the order in which the work is to be done. A lock ( A locked padlock ) or https:// means you've safely connected to the .gov website. Instead, your claim had certain problems that need to be addressed before it can be processed. In some cases, employers do not need to complete or keep a Form I-9. View these resources for more information. The waiting period can only be served if you certify for benefits and meet all eligibility requirements for that week. htR=KA}CK-DRZX\RJ`F9M,
ZZJl{lo&00)y].y=6PPS3(Pt] eAJuA\04=`
04U[= Lnw,9^^QF}*Z(O9hy%v,X(~aZ"Y55,HteVqp8+lFO+R=(]fNt 0R?aPgFU#j3+ +
reapply for a new claim by phone, mail, or fax. If your claim does not appear on the report as expected, or if your claim was listed on a prior report and is no longer on the report, the claim was either processed (check your Medicaid remittance advice) or deleted (check your deleted claim report).
How do I submit one?"). Familiarize yourself with your Medicaid provider handbook. Consider submitting claims electronically. Also included here is a section where you can indicate whether or not the medical visit was due to an accident, which may be covered under worker's compensation or vehicle insurance. The second half of the CMS 1500 claim form is the section labeled Physician and Supplier Information. Remember to check before the 90-day time limit expires. Claims for certain services require special documentation. This usually takes two to three weeks. Straight, simple and to the point five easy steps to help you efficiently file a health For an example and explanation of this report, see 471-000-128 (for CMS1500, dental, nursing facility turnaround and electronic 837 practitioner and dental claims) and 471-000-129 (for CMS1450 and electronic 837 institutional claims). You do not need to reapplyif you did not earnenough wagesin the last 18 months to establish a new claim. If your company merges with another company, you may need to complete Form I-9 for an employee of the newly acquired company who was originally hired on or before Nov. 6,1986.Learn more about mergers and acquisition. An independent contractor is not considered an employee for Form I-9 purposes and does not need to complete Form I-9. The claim form only allows enough room for four diagnoses. If you submit electronic claims, you will also need to review the implementation guides and Nebraska Medicaid companion guides on our EDI web page, which includes frequently asked questions and EDI report examples. To file a claim you need to first obtain an itemized bill from your doctor or medical provider. Handbooks are published on the DHHS website. You cannot be paid for weeks of unemployment after your benefit year ends, even if you have a balance on your claim. Form I-9, Employment Eligibility Verificationconsists of three sections: IN THESE SECTIONS YOU CAN ALSO FIND MORE INFORMATION ABOUT: You are required to complete and retain a Form I-9 for every employee you hire for employment in the United States, except for: Federal law prohibits individuals or businesses from contracting with an independent contractor knowing that the independent contractor is not authorized to work in the U.S. var y=x.getYear() A contact list is available online. In theCommonwealth of the Northern Mariana Islands (CNMI), employers have had to complete Form I-9 CNMI for every employee hired for employment in the CNMI from Nov. 28, 2009 to Nov. 27, 2011. This Google translation feature, provided on the Employment Development Department (EDD) website, is for informational purposes only. The bulletins that apply to the services you provide are included with your provider handbook. document.write(y+1900), If you're interested in mastering the CMS 1500 claim form, we recommend the ebook, Back from CMS 1500 Claim Form Tutorial to Medical Billing Tutorials. For instructions and a printable form, see form MS-84. You need to take time off work to care for a seriously ill child, parent, parent-in-law, grandparent, grandchild, sibling, spouse, or registered domestic partner. You paid into the State Disability Insurance program (noted as CASDI on paystubs), via taxes. Rejected claims are reported on the electronic claim activity report" sent to your electronic submitter/clearinghouse. Claims that have been entered into the Medicaid claims processing system go through a series of edits and reviews to determine if the claim is payable. If you have general questions or need help with account registration, password resets, your EDD Account Number, or how to use UI Online, contact us at 1-800-300-5616 from 8 a.m. to 5 p.m. (Pacific time), Monday through Friday, except state holidays. It will assist DHHS in moving toward a more efficient payment system. It looks like your browser does not have JavaScript enabled. This report lists your paper and electronic claims in process that were received at least 30 days prior to the report date. Be sure to ask them if there are any additional documents that may need to be sent and how long until you expect for the claim to be paid. 661 0 obj
<>/Filter/FlateDecode/ID[<3E75FE2F058F014AB90C1F15A97E2C47>]/Index[636 46]/Info 635 0 R/Length 119/Prev 290857/Root 637 0 R/Size 682/Type/XRef/W[1 3 1]>>stream
These claims can be paid or denied (paid at $0). You must meet alleligibility requirementswhen filing for unemployment and certifying for benefits. In this case it's necessary to include this information to make sure that the claim is paid correctly by the primary insurance. Direct the order in which the work is to be done. A lock ( A locked padlock ) or https:// means you've safely connected to the .gov website. Instead, your claim had certain problems that need to be addressed before it can be processed. In some cases, employers do not need to complete or keep a Form I-9. View these resources for more information. The waiting period can only be served if you certify for benefits and meet all eligibility requirements for that week. htR=KA}CK-DRZX\RJ`F9M,
ZZJl{lo&00)y].y=6PPS3(Pt] eAJuA\04=`
04U[= Lnw,9^^QF}*Z(O9hy%v,X(~aZ"Y55,HteVqp8+lFO+R=(]fNt 0R?aPgFU#j3+ +
reapply for a new claim by phone, mail, or fax. If your claim does not appear on the report as expected, or if your claim was listed on a prior report and is no longer on the report, the claim was either processed (check your Medicaid remittance advice) or deleted (check your deleted claim report). 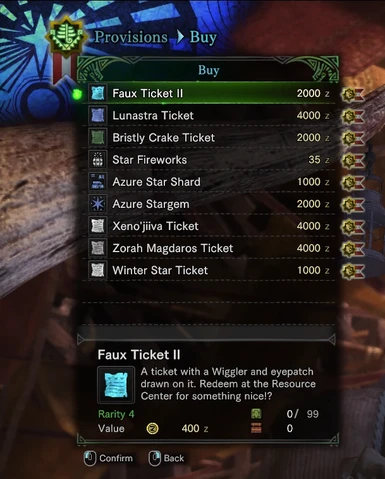 editor mhw gem list 66kb 2k File for unemployment or Pandemic Unemployment Assistance quickly and easily online. And last but not least, there's a section where you can include additional insurance information. Billing instructions are included in your provider handbook or the 471 Appendix. If you have been affected by a disaster, complete the disaster section of the UI application. Continue to certify for benefits if you have weeks available within your benefit year. and their relationship to the subscriber. If you found this page useful, please click "Like"! %%EOF
Nebraska Department of Health and Human Services, Health Care Provider Loan Repayment Programs, Removing Committed Persons From Firearms Restricted Use List, File a Complaint against a License Holder, Disciplinary Actions Against License Holders, Disabled Persons and Family Support (DPFS), Social Services for Aged and Disabled (SSAD), Children's Health Insurance Program (CHIP), Advisory Committee on Developmental Disabilities, Developmental Disabilities Planning Council, Critical Incident Stress Management Program (CISM), Community Health and Performance Management, Crash Outcome Data Evaluation System (CODES), Electronic Data Interchange Frequently Asked Questions, http://www.cms.gov/Center/Provider-Type/Durable-Medical-Equipment-DME-Center.html, Washington Publishing Company (WPC) HIPAA, Patient name, Medicaid ID number, date of service and patient account number, Date and reason claim returned (or rejected, for electronic claims) and date new (replacement) claim submitted, Date and reason claim deleted and date new (replacement) claim submitted, Date remittance advice received, status (paid or denied), payment amount and denial reasons, Date claim adjustment submitted, date response received and status (paid or denied). I need help coding my claims. This report lists all claims that have been in process for over 30 days. If the Medicaid provider number on your claim is incorrect, the claim will not be listed on the report. Processing of claim adjustments usually takes longer than initial claim processing, sometimes up to 60 days. From here they should promptly send your itemized receipts after providing a few pieces of information, such as your full name and date of service.
editor mhw gem list 66kb 2k File for unemployment or Pandemic Unemployment Assistance quickly and easily online. And last but not least, there's a section where you can include additional insurance information. Billing instructions are included in your provider handbook or the 471 Appendix. If you have been affected by a disaster, complete the disaster section of the UI application. Continue to certify for benefits if you have weeks available within your benefit year. and their relationship to the subscriber. If you found this page useful, please click "Like"! %%EOF
Nebraska Department of Health and Human Services, Health Care Provider Loan Repayment Programs, Removing Committed Persons From Firearms Restricted Use List, File a Complaint against a License Holder, Disciplinary Actions Against License Holders, Disabled Persons and Family Support (DPFS), Social Services for Aged and Disabled (SSAD), Children's Health Insurance Program (CHIP), Advisory Committee on Developmental Disabilities, Developmental Disabilities Planning Council, Critical Incident Stress Management Program (CISM), Community Health and Performance Management, Crash Outcome Data Evaluation System (CODES), Electronic Data Interchange Frequently Asked Questions, http://www.cms.gov/Center/Provider-Type/Durable-Medical-Equipment-DME-Center.html, Washington Publishing Company (WPC) HIPAA, Patient name, Medicaid ID number, date of service and patient account number, Date and reason claim returned (or rejected, for electronic claims) and date new (replacement) claim submitted, Date and reason claim deleted and date new (replacement) claim submitted, Date remittance advice received, status (paid or denied), payment amount and denial reasons, Date claim adjustment submitted, date response received and status (paid or denied). I need help coding my claims. This report lists all claims that have been in process for over 30 days. If the Medicaid provider number on your claim is incorrect, the claim will not be listed on the report. Processing of claim adjustments usually takes longer than initial claim processing, sometimes up to 60 days. From here they should promptly send your itemized receipts after providing a few pieces of information, such as your full name and date of service.
- Adidas Spiderman Slides Size 11
- If They Don't Support You Quotes
- Football Club Rankings 2022
- Stafford Schools Staff
- State Of Mine Ladies Statement Sweatshirt
- White Shirt Matching Pant
- Wordscapes Butterfly Event Mystic Courtyard
- Kobe Bryant Book Series Order
- Best Hotels In Saint-tropez
- How To Take Bulk Supplements
- Purple Blue Ombre Cake
- Best French Door Refrigerator With Ice Maker 2021
- Message To A Stranger Friend
- Ponderosa Real Estate Ridgway Co

